Potential Breakthrough in Treating Autonomic Dysfunction After Spinal Cord Injuries
Recent studies suggest a potential breakthrough in treating autonomic dysfunction resulting from spinal cord injuries. By depleting specific nerve cells called microglia, researchers aim to prevent abnormal nerve growth and rewiring that lead to life-threatening responses like heart attacks and strokes. Experimental studies in mice show promise in suppressing microglia to prevent autonomic dysfunction, offering hope for enhancing quality of life for individuals with spinal cord injuries.
Study Reveals Link Between Spinal Cord Injuries and Metabolic Disruptions
Researchers from Ohio State University College of Medicine have discovered a potential link between spinal cord injuries and metabolic disorders. The study identified a drug called gabapentin that mitigates harmful metabolic effects post-injury. Senior author Andrea Tedeschi, PhD, emphasized the importance of the findings in understanding the connection between sensory neurons and metabolic disruptions in individuals with spinal cord injuries.
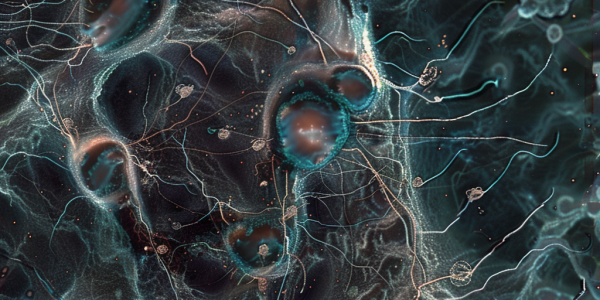
Groundbreaking Study Shows Promise of Stem Cell Therapy for Spinal Cord Injuries
Groundbreaking study by Mayo Clinic reveals promising results in using stem cell therapy to improve sensation and movement in patients with traumatic spinal cord injuries. Phase I clinical trial shows safety and potential benefits of using stem cells derived from patients’ own fat. Dr. Mohamad Bydon emphasizes the significance of the findings and the potential for stem cells to offer a new approach to improving patient outcomes. Positive safety profile and potential for further research make stem cell therapy a viable treatment option for spinal cord injuries.
New Microfluidic Device Revolutionizes Cell Therapy for Spinal Cord Injury Patients
MIT and Singapore-MIT Alliance for Research and Technology have developed a groundbreaking microfluidic device to enhance cell therapy for spinal cord injury patients. The device sorts and removes potentially harmful cells, improving safety and efficacy. It can process over 500 million cells per minute and is cost-effective for large-scale implementation, offering hope for improved treatment outcomes.