New Insights into Glioblastoma: Understanding Tumor Cell Integration into Brain Circuits
Recent research from Heidelberg University and its associated institutions has unveiled significant findings regarding the behavior of glioblastoma cells, particularly their integration into brain-wide neuronal circuits. This groundbreaking study, published in the journal Cell, highlights the complex interactions between aggressive brain tumors and nerve cells, shedding light on potential avenues for future therapies.
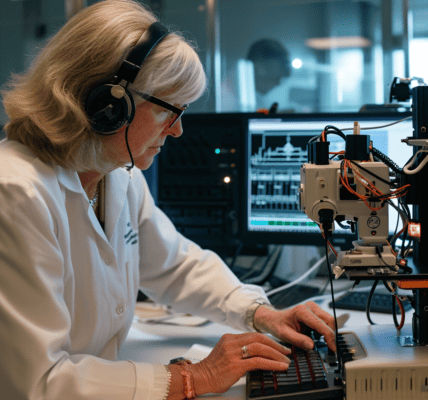
Glioblastomas are notorious for their aggressive nature and ability to infiltrate brain tissue, making them one of the most challenging types of brain cancer to treat. The research team, led by Dr. Varun Venkataramani, utilized a novel mapping technique involving modified rabies viruses to observe how glioblastoma cells interact with nerve cells in both human tissue models and mouse brains.
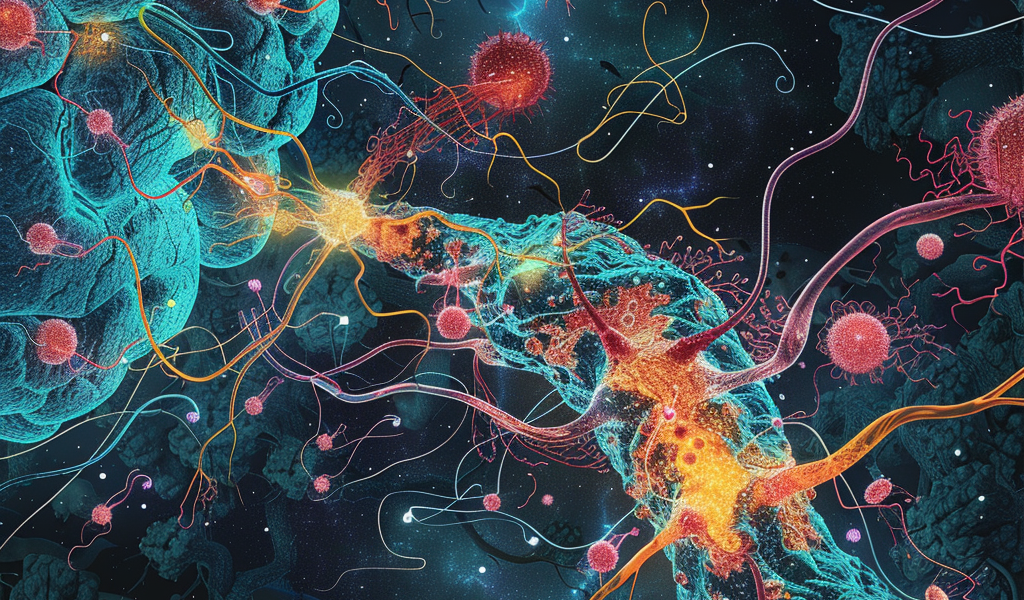
The findings indicate that glioblastoma cells extend their reach into the brain, resembling a mycelium network. This invasive behavior is significantly influenced by the nerve cells, which form direct connections with the tumor cells and transmit excitatory signals that promote tumor growth. The study reveals that these interactions occur much earlier in the disease process than previously understood and involve a broader range of nerve cell types.
Dr. Venkataramani’s innovative approach involved infecting and labeling human glioblastoma cells with modified rabies viruses. This method allowed the researchers to track the spread of the virus from tumor cells to contact-seeking nerve cells. The rabies virus, known for its ability to infect nerve cells, serves as a powerful tool for understanding the dynamics of glioblastoma invasion.
Professor Dr. Wolfgang Wick, Medical Director of the UKHD’s Department of Neurology, emphasized the implications of these findings, stating, “The tumor network makes glioblastomas so difficult to fight: they cannot be completely removed, and their interconnection makes them almost insensitive to radiation and chemotherapy.” This highlights the critical need for ongoing research to uncover the mechanisms that underpin glioblastoma’s resilience against current treatment modalities.
Despite advancements in therapeutic strategies, glioblastoma patients face a grim prognosis, with an average survival rate of less than two years following diagnosis. The study’s insights into the tumor’s intricate network and its interactions with the brain’s neuronal circuitry provide valuable information that could lead to the development of more effective treatment options.
The research employed a dual labeling approach, allowing for the investigation of both individual glioblastoma cells and the broader neuronal connectome associated with the tumor. This dynamic investigation is crucial for understanding how glioblastoma cells establish connections within the brain, facilitating their growth and resistance to treatment.
As the scientific community continues to explore the complexities of glioblastoma, this study represents a significant step forward in identifying potential weak points in tumor behavior. By understanding how glioblastoma cells communicate and integrate with the brain’s neuronal networks, researchers hope to pave the way for innovative therapeutic strategies that could improve patient outcomes.
In summary, the recent study from Heidelberg University offers a fresh perspective on the interactions between glioblastoma cells and the brain’s neuronal circuits. With the potential for new therapeutic approaches on the horizon, continued research in this area is essential for combating one of the most aggressive forms of brain cancer.