Scientists have made a groundbreaking discovery in the genetic pathway of neuroblastoma, a childhood cancer, providing new possibilities for personalized treatments. Researchers from the University of Sheffield have developed a stem cell model to delve into the origins of neuroblastoma, a cancer that predominantly affects infants and young children.
Neuroblastoma, the most common childhood tumor outside the brain, impacts around 600 children in the European Union and the United Kingdom annually. Understanding genetic changes and their impact on neuroblastoma initiation has been challenging due to the lack of suitable laboratory techniques.
However, a new model created by the University of Sheffield researchers, in collaboration with the St Anna Children’s Cancer Research Institute in Vienna, has successfully replicated the emergence of early neuroblastoma cancer-like cells, providing valuable insights into the genetic pathway of the disease.
The research, recently published in Nature Communications, has unveiled the intricate genetic pathways that trigger neuroblastoma. The international research team identified that specific mutations in chromosomes 17 and 1, coupled with the overactivation of the MYCN gene, significantly contribute to the development of aggressive neuroblastoma tumors.
Childhood cancer is often diagnosed late, leaving researchers with limited knowledge of the conditions leading to tumor initiation, which occurs early during fetal development. To comprehend tumor initiation better, it is crucial to have models that recreate the conditions precipitating tumor formation.
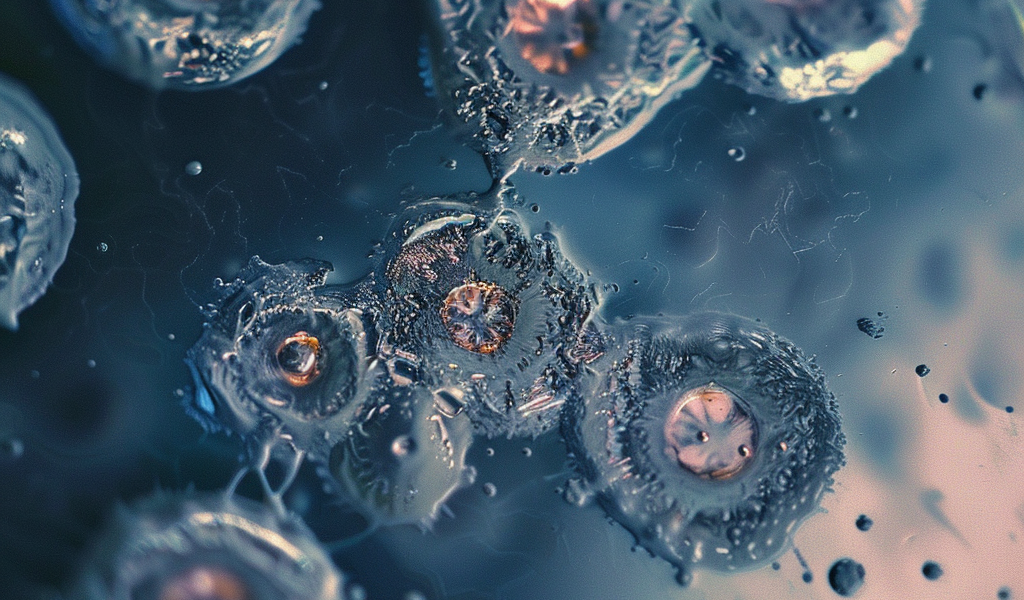
Neuroblastoma typically originates in the womb when a group of normal embryonic cells known as ‘trunk neural crest (NC)’ undergo mutations and become cancerous. Through an interdisciplinary effort led by stem cell expert Dr. Ingrid Saldana from the University of Sheffield and computational biologist Dr. Luis Montano from the St Anna Children’s Cancer Research Institute, the study utilized human stem cells to cultivate trunk NC cells in a petri dish.
These cells exhibited genetic alterations commonly observed in aggressive neuroblastoma tumors. By employing genomics analysis and advanced imaging techniques, the researchers observed that the modified cells began to exhibit cancer-like behavior, resembling neuroblastoma cells found in afflicted children.
These findings present a promising avenue for developing tailored treatments that target the cancer specifically while minimizing the adverse effects associated with current therapies. The stem cell-based model developed by the researchers mimics the early stages of neuroblastoma, offering hope for more effective and personalized treatment strategies in the future.