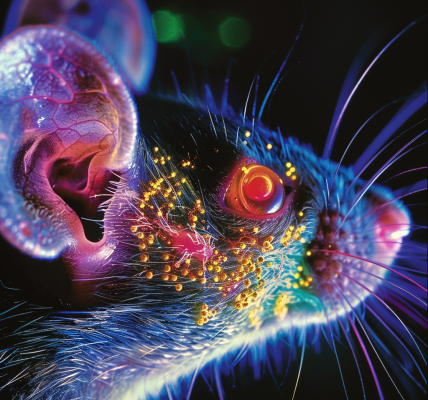
An important aspect of aging is how the immune system changes over time, which has consequences and contributes to the greater risk for severe infections and other diseases such as cancer in the aging population. Researchers at The Jackson Laboratory (JAX) and UConn Health are rigorously investigating why vaccines don’t work as well in some older adults.
Streptococcus pneumoniae is a dangerous bacterial pathogen that causes diseases such as pneumonia, meningitis, and sepsis. Infants and older adults are at the greatest risk for pneumococcal infections, and case-fatality rates increase with age for reasons still not well understood.
Several vaccines developed against the polysaccharides found on the surface of S. pneumoniae, including PPSV23 (Pneumovax), are generally effective in older adults, though not as protective as in younger adults. Combining the polysaccharide with a protein, such as a nontoxic variant of a diphtheria toxin, can induce additional adaptive immune activation, resulting in better protection.
The strategy was used to develop a new class of FDA-approved conjugated vaccines (e.g., PCV13, Prevnar). Despite these advances, responses to pneumococcal vaccines still decline with age. Moreover, it remains unclear which of these two vaccines are preferable in subpopulations of older adults.
To address these gaps in knowledge, a team led by JAX Associate Professor Duygu Ucar, Ph.D., UConn Health Professor and Director of UConn Center on Aging George Kuchel, M.D., C.M., and Jacques Banchereau, Ph.D. (Immunoledge, Montclair, NJ), recruited and vaccinated a cohort of 39 pneumococcal vaccine-naïve healthy adults, all aged 60 or above, to thoroughly compare pre- and post-vaccine immune characteristics.
Their findings, presented in ‘Distinct baseline immune characteristics associated with responses to conjugated and unconjugated pneumococcal polysaccharide vaccines in older adults,’ published in Nature Immunology, identify the biological traits underlying variable responses to the two different vaccines. Importantly, they also reveal distinct baseline (i.e., pre-vaccination) predictors that have the potential to affect vaccination strategies and lead to interventions that are more effective, by virtue of being more specific.