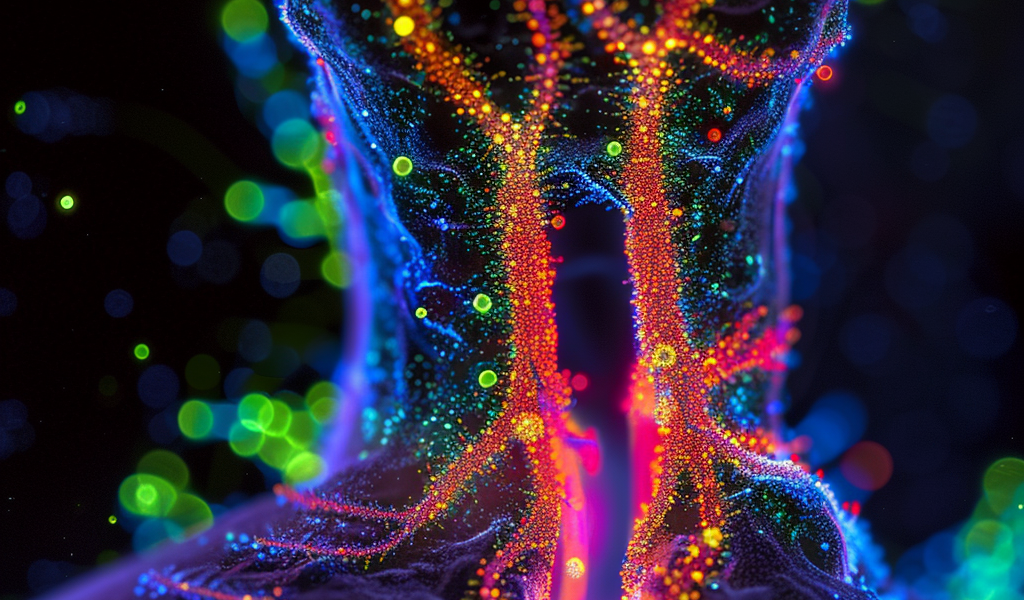
A groundbreaking discovery has been unveiled by researchers, revealing a direct communication between the lungs and the brain when an infection occurs. This mechanism alters the traditional understanding of sickness response, as it demonstrates that neurological pathways, rather than just immune responses, are responsible for the symptoms of illness.
The study, conducted in mice, found that the lungs utilize neurons involved in the pain pathway to alert the brain about infections, leading to symptoms of sickness through nervous system activation rather than solely through the immune response. This direct lung-brain communication has significant implications for the treatment of respiratory infections and chronic lung conditions, as it opens possibilities for dual treatment strategies that address both the infection and its neurological impact.
Dr. Bryan Yipp, a clinician researcher at the Cumming School of Medicine and senior author of the study, emphasized the significance of the findings. According to Dr. Yipp, the brain plays a critical role in triggering the symptoms of sickness, prompting the overall feeling of being unwell, tiredness, and loss of appetite. This discovery indicates that treating respiratory conditions may require addressing the nervous system as well as the infection.
Prior to this study, it was believed that infections in the lungs and pneumonia induced inflammatory molecules that eventually reached the brain through the bloodstream, leading to sickness as a consequence of the immune system kicking into action. However, the new findings reveal that sickness actually results from nervous system activation in the lung, challenging previous assumptions about the mechanisms underlying illness.
Moreover, the study observed gender differences in sickness behavior, with male mice showing more severe symptoms than females under the same conditions. This suggests that neuronal communication plays a more significant role in males, shedding light on gender disparities in illness experiences.
The University of Calgary researchers behind the study have shed light on the critical role of the brain in sickness response, offering new insights that may revolutionize the way respiratory infections and chronic lung conditions are treated. By understanding the lung-brain dialogue, the potential for better management of these conditions through comprehensive treatment strategies that target both the infection and its neurological impact is on the horizon.